Cover Story: Taking it to the Streets
Understanding that healthcare doesn’t only exist within the walls of medical facilities, Hartford HealthCare has long been bringing care to the communities and people we serve even before the COVID-19 pandemic struck and starkly highlighted the gaps in access to care and with care experiences.
The work — accelerated by the pandemic’s demand for COVID testing and vaccination — coincided with the system’s amplified diversity, equity, inclusion and belonging (DEIB) efforts which prompted us to meet our patients where they are, in all ways. This includes rebuilding trust in the American healthcare institution that mistreated many minorities through the years, and mobilizing efforts to reach people living in areas, both inner city and rural, where quality healthcare has been nonexistent.
There are shiny new CareVans traversing the capital and northwest regions, there are clinics and support groups conducted in Spanish, there are special events tailored to the underserved and disenfranchised and food distribution targeting the dietary requirements of specific diseases. It happens every day at Hartford HealthCare, in every region.
—Susan McDonald
Valuing Equity
Susan McDonald
The events of 2020 prompted Hartford HealthCare to examine its values and adopt a new one — “Equity, We do the just thing.”
While one word might seem insignificant, the addition — adopted over the summer after approval from the board of directors — is momentous, made thoughtfully, with input from colleagues across the system.
The words that proclaim our values serve as both a mirror reflecting who we are and a compass guiding us to what we aspire to be. The word — like Safety, Caring, Excellence and Integrity — is a challenge that we, after all we’ve experienced, are ready to face.
Perhaps Equity has always been present, embedded in each of the other four Values. But calling it out as a Value itself and using it as a measuring stick for progress as our Diversity, Equity, Inclusion & Belonging (DEIB) efforts across the system expand and yield change is how we can generate momentum and celebrate success.
Like our other Values, living up to our Equity promise will be difficult and occasionally cause us to see and think differently as we prioritize curiosity over judgment, improvement over discomfort, action over words. Therein lies the challenge and the reward.
Hartford HealthCare has been guided by four legacy Values since formation. The new one, Equity, will guide us as we provide an even better level of care and compassion for those we serve.
East Region
Elissa Bass
East Region colleagues actively engaged with communities on more than just getting COVID vaccine into arms, although they certainly took vaccine into homes, schools and even onto a farm. Efforts include:
- Using an apartment in Willimantic’s 444-unit Colonial Townhouse Apartments, colleagues created a clinic with North Central and Eastern Highlands health districts and Access Community Action Agency.
- Hosting a vaccine clinic at Windham Heights, low-income apartments in Willimantic, that attracted 75.
- Registering more than 70 Groton high school students for the vaccine through the schoolbased health clinic. Parents like Heather Hanson, who came to sign consent for her 16-year-old, Kimberly, could also be vaccinated. Getting the vaccine, the teen softball player said, “makes me happy. I’m so excited to get back to normal.”
- Partnering with the state Department of Public Health and United Way of Southeastern Connecticut on the “Trusted Messenger Program” fighting vaccine hesitancy. More than 30 representatives from New London County social service departments, private nonprofits and others gathered to hear how to effectively talk to clients about COVID vaccines and gather resources to schedule appointments.
- Sponsoring the Windham County Latino Fest, bringing HHC providers and colleagues to downtown Willimantic to distribute information about such services as bariatrics, cardiac health, movement disorders and women’s health. A mobile vaccine clinic was stationed just inside the gates, and three Zumba classes were taught.
- Connecting with Pawcatuck Neighborhood Center (PNC) in Stonington to provide tailored food boxes to PNC food pantry clients with specific health issues like diabetes or heart disease. Community health teams trained PNC volunteers to pack boxes with beneficial foods, recipes and health information.
- Expanding Backus Hospital’s longtime farm stand to Windham Hospital, with weekly sessions from July through fall. The Healthy Rx Program also expanded to Windham, giving nutritionally at-risk families vouchers toward the purchase of fresh fruits and veggies at the farm stand.
 Backus Registered Dietitian Katie Field, right, checks the ingredients of some popular cereals with Pawcatuck Neighborhood Center volunteer Jack Jacobs. Field taught volunteers about food choices specific to several health conditions, including kidney disease, heart disease and diabetes as part of a collaborative program between Hartford HealthCare and the center to provide information about healthy food choices to families served by the Center’s food pantry.
Backus Registered Dietitian Katie Field, right, checks the ingredients of some popular cereals with Pawcatuck Neighborhood Center volunteer Jack Jacobs. Field taught volunteers about food choices specific to several health conditions, including kidney disease, heart disease and diabetes as part of a collaborative program between Hartford HealthCare and the center to provide information about healthy food choices to families served by the Center’s food pantry.
Photo by Jeff Evansd
Central Region
Brian Spyros
Central Region colleagues are fully committed to the communities served and recognize that commitment often needs to go beyond the confines of our hospitals to reach people where they live and work. Efforts include:
Supporting diversity, equity and inclusion programs such as the Juneteenth Celebration at the New Britain Museum of American Art.
Working closely with the Opportunities Industrialization Center, the oldest employment and training program in New Britain, on opportunities for out-of-school youth, age 18 to 24, to gain work experience. The Hospital of Central Connecticut does the same for New Britain High School students wanting to work in healthcare, creating a career channel with our clinical colleagues.
After racial injustice was deemed a public health issue, collaborated with the Liberty Bank Foundation through the Meriden Provider Network on Racial Justice and Links Inc. to help provide mental health education to communities of color.
Strengthening relationships with our community partners — local YMCAs, chambers of commerce, churches and schools — during the COVID-19 pandemic to share information and updates. When vaccine rollout began in January 2021, that outreach was again critical in ensuring people had correct information and knew where to get vaccinated. This was done through media coverage, social media interviews, Zoom meetings, presentations and discussion with our providers. The Central Region Executive Leadership Team worked closely with area health departments to address vaccine hesitancy, especially in Black and Latinx communities.
Bringing vaccine into communities and neighborhoods identified as having low vaccination rates, as part of our mission to make sure everyone who wants the vaccine has access to it. Micro and mobile clinics have stopped at the Spanish Health Council of Wallingford, Curtis Cultural Center and John Barry Elementary School in Meriden, Wallingford and Southington YMCAs, Plainville Recreation Department and even restaurants to reach hospitality workers. Some clinics were promoted through boots on the ground outreach with colleagues going to stores, churches and businesses to hand out flyers with vaccine information.
 Many COVID-19 vaccinations were distributed through a mega vaccine clinic at One Liberty Square in New Britain.
Many COVID-19 vaccinations were distributed through a mega vaccine clinic at One Liberty Square in New Britain.
Photo by Rusty Kimball
Behavioral Health Network
Robin Stanley
By nature of the work they do, colleagues at the Behavioral Health Network (BHN) are often working in communities around the state. Outreach efforts include:
Working to combat the opioid crisis in partnership with the Meriden Health Department to develop the Meriden Opioid Referral for Recovery program (MORR). Funding comes through a Substance Abuse and Mental Health Services Administration grant. MORR connects members of the community who have experienced overdose or opioid-related emergency with Rushford clinicians to facilitate access to treatment and other resources they may not otherwise receive. Since Rushford first began this partnership in 2018, 150 people who overdosed in Meriden have been connected to treatment. MORR teams meet people where they are and work to prevent the cycle of overdose, hospitalization, jail time or worse. A Rushford clinician is often the first person patients see at their bedside after waking up from an overdose, and clinicians often go on ride-alongs with police to help intervene in the moment.
Starting the Meriden Early Diversion, Referral and Retention (MERR) program with the Meriden Police Department and Department of Health and Human Services. The grant-funded diversionary program gives police officers an additional resource when an arrest may be avoided and the person better served by participating in intensive mental health or crisis intervention treatment through Rushford. The program brings help those who otherwise could get lost in the cycle and miss an opportunity for recovery.
Launching the Purple Light Project to raise money for psychiatric patients in the Hartford Hospital Emergency Department. Led by Erica Moura, manager of the Institute of Living Assessment Center, the Purple Light Project is so named for the purple pod psychiatric section of the ED where the light is always on for anyone suffering from a mental health crisis. It was initially launched to make the purple pod more humane and patient-centered and bring awareness and community support for mental health needs.
In its first year, the Purple Light Project raised more than $20,000 for warm winter clothing, food, hygiene products, blankets and taxi or bus vouchers for patients. The Purple Light Project now supports all seven of the system’s emergency psychiatric locations. This year, through an online auction and the first Purple Light Project 5K, more than $53,000 was raised.
 Jessica Matyka, clinical director of Rushford, spoke at a summer press conference at the Meriden Police Department about the city’s partnership with Rushford and the Behavioral Health Network to offer the Meriden Opioid Referral for Recovery program.
Jessica Matyka, clinical director of Rushford, spoke at a summer press conference at the Meriden Police Department about the city’s partnership with Rushford and the Behavioral Health Network to offer the Meriden Opioid Referral for Recovery program.
Hartford HealthCare at Home
Ken Harrison
As a crew from Japanese Television New York rolled film, the Hartford HealthCare at Home (HHAC) team celebrated delivering its first dose of the COVID-19 vaccine into the arm of 92-year-old Manchester resident Edna Hennessey.
“This is super hero stuff we are doing,” said Bridget Kennedy, HHAC clinical team manager. “It’s an amazing feeling to be a part of the solution,” echoed Kristen Murphy, HHAC regional director of operations.
The pair and their team prepared doses and a schedule for distributing them to clients who, for a variety of health-related reasons, cannot leave their homes to visit a vaccine clinic.
“We are excited to be able to provide this service for our patients who are most vulnerable and at risk,” said Courtney Weyel, RN who gave Hennessey her shot at home.
Sitting comfortably in the living room of the house where she has lived for the past 71 years, Hennessy smiled beneath her mask and rolled up her sleeve. She has a family history with pandemics — her father lost his first wife and infant son to the Spanish Flu, so the magnitude of the moment was not lost on her.
She repeatedly thanked Weyel, saying they were “going above and beyond.”
When asked what she looked forward to most when fully vaccinated, Hennessy glanced thoughtfully at the photos adorning the fireplace mantle.
“Seeing my grandchildren and greatgrandchildren in person again. I can’t wait for that,” she said.
 Edna Hennessey was able to get her COVID-19 vaccine in the comfort of her Manchester home, courtesy of Courtney Weyel, RN, from Hartford HealthCare At Home.
Edna Hennessey was able to get her COVID-19 vaccine in the comfort of her Manchester home, courtesy of Courtney Weyel, RN, from Hartford HealthCare At Home.
Northwest Region
Tim Lebouthillier
In the more rural Northwest Region of the state, the community’s needs mirror those in more urban areas, and the efforts of Charlotte Hungerford Hospital teams work to address them with various services and initiatives. These include:
- Launching, in February 2021, of a team of community partners and “vaccine ambassadors” to connect with underserved populations, underserved neighborhoods, and people living in senior centers and public housing sites.
- Creating a “health equity” clinic in a trailer outside the Emergency Department to provide COVID-19 vaccine and other health services for 12 straight Wednesdays. Translators from New Opportunities helped patients and providers communicate seamlessly, and transportation was provided by the local Senior Center.
- Providing vaccines through pop-up sessions in congregate living areas, schools, camps, businesses, town halls, soup kitchens and for homebound patients. More than 2,000 people were vaccinated through these health equity efforts.
- Coordinating the Produce RX Program which distributed 16 weeks of fresh produce, with nutrition and other wellness information, to 50 families.
- Partnering with the NW CT Healthy Eating and Active Living Initiative to offer physical activities and nutrition education programs for all ages, both in-person and virtual.
- Installing 20 bike racks around Winsted and Torrington.
- Hosting a three-day Diabetes Boot Camp retreat for diabetic patients, in collaboration with the Neighborhood Health Initiative.
 Carla Angevine, manager of community health and health promotion in the Northwest Region, and executive director of Fit Together, poses with a bike rack installed along the Sue Grossman Stillwater Greenway in Torrington. Photo by Jessica Stewart
Carla Angevine, manager of community health and health promotion in the Northwest Region, and executive director of Fit Together, poses with a bike rack installed along the Sue Grossman Stillwater Greenway in Torrington. Photo by Jessica Stewart
Hartford Region
Brenda Kestenbaum
In the heart of the state, Hartford may seem close to quality healthcare, but some neighborhoods and cultural groups might as well be miles away. A variety of outreach efforts, however, seek to bring care closer to home for residents. These include:
- Partnering with Woman’s Ambulatory Health Services and Hartford HealthCare’s Early Detection and Prevention Program, Hartford Hospital held a Women’s Wellness Day, offering free services like clinical breast exams, PAP smears and HPV tests. Cholesterol screenings and physical activity assessments helped identify patients at risk for heart disease, stroke or other cardiovascular disease. On-site screenings were offered for early detection of breast and cervical cancer, including mammograms on the system’s mobile mammogram vehicle.
- Presenting a series of webinars on the topic “Colon Cancer in the Black Community” in recognition of Colon Cancer Awareness Month and inviting members of the local Black fraternities and organizations. The webinars offered participants a chance to discuss colon cancer signs and symptoms with providers.
- Engaging members of underserved communities in Hartford on the importance of COVID-19 vaccination. Vice President of Community Health Greg Jones took to Facebook Live to reach people to stress access to vital services in urban areas. The series of live videos brought the message to people where they were and served as an important vehicle to getting the message out.
- Opening a 3,000-square-foot, state-of-the-art Community Pharmacy at Hartford Hospital which expanded service for patients, community residents and colleagues. Free delivery is available for residents in the community and the “Meds to Beds” service provides medication and prescriptions to patients before they are discharged from the hospital.
- Deploying members of the Northern Connecticut Black Nurses Association, co-founded by Hartford Hospital Nurse Educator Marlene Harris, RN MSN, across underserved areas, distributing masks, demonstrating their proper use and providing smaller children’s masks. The group’s presence in the community is deep-seeded. “We have a great collaboration with the hospital and work hard to provide things like blood pressure screenings and other services to the community,” Harris shared.
Photos: Right: Hartford Hospital staff came together to donate food and supplies to My Sisters Place in Hartford, while Hartford Hospital advanced practitioners served meals at the shelter. Left: In partnership with Foot Wear With Care, the State of Connecticut and the Hartford Police Department, Hartford HealthCare providers participated in a free clinic providing Johnson & Johnson COVID-19 vaccines and free sneakers for homeless persons at the Band Shell at Bushnell Park in Hartford.
Fairfield Region
St. Vincent’s Medical Center has a 115-year history of addressing health disparities and our founding was predicated on addressing a fundamental health disparity in the Bridgeport. In 1903, there was one hospital in the city and the only people who could be treated there were White Anglo-Saxon Protestants. A group of doctors wanted a hospital that would treat everyone and invited the Daughters of Charity to open one. Our very founding and essence has been an attempt to address health disparities and equity. Recent examples include:
- Coordinating the Hope Dispensary of Greater Bridgeport, a free pharmacy serving those without access to life-saving medications. In fiscal year 2020, Hope filled 11,337 prescriptions, which would have cost patients more than $1 million if they had to be filled at a commercial pharmacy.
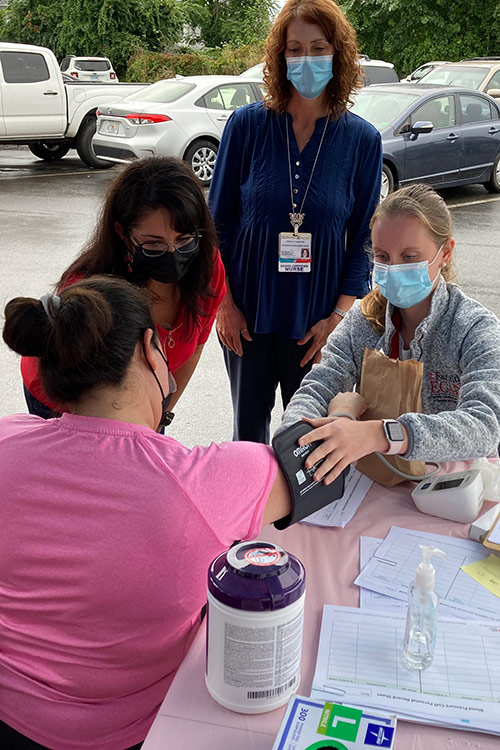
St. Vincent’s Medical Center Parish Nurse Coordinator Marilyn Faber, RN, supervises Fairfield University nursing students alongside Professor Jessica Planas, as they conduct blood pressure screenings at Hope Dispensary.
- Hosting annual Medical Mission at Home events, providing a full array of medical, behavioral health, foot washing and podiatry services to medically underserved in our community. This annual event provides services to more than 400 community members and allows almost 500 colleagues to actively participate in living our core values.
- Convening the Health Improvement Alliance for 15 years. This community collaborative brings together two hospitals, two health centers, seven health departments, and more than 100 community partners to conduct the Community Health Needs Assessment and develop and implement the Community Health Plan addressing unmet medical needs in underserved populations. This work reaches far into the community and delivers services to food pantries, soup kitchens and substance abuse programs. Services include diabetes and blood pressure screenings, nutritional counseling, assistance in healthy food selection, farmers markets, monthly food distribution, and activities to promote healthy lifestyles and communities.
- Bringing COVID-19 vaccinations to more than 50,000 at two mega sites, our retail pharmacy and mobile community clinics. Collaborating with the state, local health departments and community partners ensured we reached deep into the community to vaccinate underserved populations.
—Danielle Swift