Behind the Scenes
Supplying ‘MORR’ expertise in the opioid crisis
By Susan McDonald
John Potter squatted in the grassy yard of a three-family Meriden home, close enough to chat with Neal, a man stretched out for what he called “a siesta.”
“Neal, why are you lying here?” Potter said gently. “Do you think you should go to the hospital?”
The Rushford clinician was riding the streets of Meriden with Police Officer Garrett Ficara as part of the Meriden Opioid Referral for Recovery (MORR) partnership when they heard about a man down. They rushed over, concerned about a possible drug overdose.
Neal consented to go to MidState Medical Center. Just a year earlier, before MORR started, Potter wouldn’t have been riding with Ficara and there would be no way to know whether people such as Neal ever made it to treatment.
“I used to feel that a lot of people get lost after we deal with them,” said Ficara, who felt called to public service after growing up with parents in healthcare. His mother, Cheryl,
is chief nursing officer and vice president of patient care services at Hartford Hospital, and his father, Robert, is a physician assistant in cardiac surgery. “A lot of people want help, but the streets take over.”
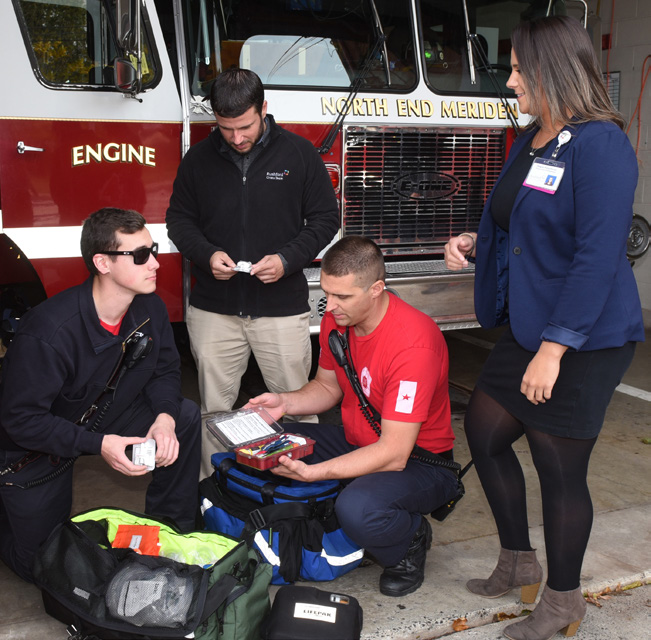
Through MORR, Meriden’s first responders are connecting people with opioid use disorder (OUD) to help at Rushford. The program, funded by a $2 million federal grant, provides first responders with training and Narcan kits to reverse opioid overdoses. Those who want treatment are connected with Rushford for services. “The purpose of the MORR project is to streamline the path to recovery for people with OUD,” said Jessica Matyka, LCSW, director of crisis services and community programs at Rushford.
In the first six months, 52 referrals to Rushford treatment programs were made by MORR teams in Meriden, an area hit hard by the opioid crisis. In addition, Matyka said Rushford’s Prevention Department has trained 117 first responders in Mental Health First Aid and six in the CIT model.
Officer Michael Shedlock said police try to be compassionate and understand that OUD often starts when people seek relief for injuries.
“They start opioids for the pain then move to heroin. Then they’re spending everything they have on it, and wind up homeless,” explained Shedlock. “It’s sad to see so many people in such bad places.”
At one fire station, Potter talks with firefighters, who are often the first on the scene of an overdose, about the challenges of using Narcan, especially when the victim has suffered repeated overdoses.
Potter and Megan Fitzsimons, a Rushford prevention professional, also visit motels to hand out business cards, teach staff to administer Narcan and talk about recovery.
“I will train your staff in a heartbeat,” he told the manager of one motel, where a woman recently overdosed. Later, he explained, “I just started going places where clients had overdosed or frequent, recognizing the need to educate on overdose or withdrawal symptoms and Narcan use. For the most part, people are receptive.”
For first responders like Ficara, MORR resources are welcomed. “Mental health is one of the biggest things we have to deal with. It really helps to have MidState and Rushford helping us,” he said. “Cops may not seem like they care, but it’s good to know that what we’re doing matters, that we’re helping people.”
Photos by Jeff Evans
The MORR team from Rushford, first photo, includes John Potter and Megan Fitzsimons. They take Narcan and other life-saving materials into the community, working closely with Meriden’s first responders and training people like women running a shelter near the downtown area how to use Narcan. The goal is to connect people with substance use disorder to Rushford’s services when they want to become sober.